Outcomes Delivered
With over 25 years of experience in healthcare and product innovation, I specialize in delivering measurable, impactful outcomes through User Experience Research and Product Management.
My expertise lies in:
- Outcomes Driven Innovation
- Product Management
- Customer Experience
- Job-to-be-Done (JTBD) framework
- Leveraging AI technologies for innovation
I ensure that outcomes drive every initiative, whether it's achieving positive results for clients, advancing research and development, or crafting user-centered products. By applying the Jobs-to-be-Done (JTBD) framework in UX research and product management, I help organizations uncover the true needs of their customers and create solutions that align perfectly with those needs.
This comprehensive method ensures that clients achieve their business goals and see real, measurable benefits from our collaboration. I'm passionate about guiding organizations towards meaningful products that align with the outcomes they and their customers want to achieve.
My approach involves:
- Identifying the core jobs customers are trying to get done
- Analyzing user experience data to understand pain points and opportunities
- Customer Experience
- Applying JTBD principles to product management strategies
- Leveraging AI to enhance decision-making and product development processes
Professional Roles
I serve as an Advanced Researcher at CVS/Aetna focused on patient outcomes and Director of Customer Experience at ADX focused on business outcomes.
Outcomes Studies
Automated Outcomes Studies
The Outcomes-Driven Innovation method is valuable because it demonstrates a rigorous, customer-focused approach to product innovation. However, it is costly and requires both quantitative and qualitative asessments. I have developed an automated method to deliver Outcomes-Driven Design using publicly available data and AI. Below are the studies I have conducted in this way.
This method allows a fast assessment of a market before committing time to a full study. It also allows directional information for markets that may be costly or impossible to recruit particpants.
Patient Outcomes Studies
Due to the inherent complexity of the issues faced by healthcare patients, defining innovation in this field presents significant challenges. However, Outcomes Driven Innovation facilitates a comprehensive, enterprise-wide approach to patient innovation.
Family Health Managers
Choose and Manage Healthcare Providers
Find a product on a retail website
Get suggestions from AI (LLM Chatbot)
Know What I Owe for a Health Care Visit
Know when a product goes on sale
Manage an Online Pharmacy Account
Navigate insurance coverage and benefits
Navigate commercial healthcare coverage challenges
Seek medical help for migraines
Get a prior authorization from your insurance for a medical treatment
Plan to pay for unexpected health events
Remember my family's preventative care
Schedule a retail health visit
Understand and manage healthcare costs
Set up payments for an ongoing service
Seek help for emotional and mental health issues
Various Studies
The studies below go beyond outcomes studies and answer questions in a variety of areas.
Use AI to Reduce Cost of Research
Can Natural Language Processing (NLP) reduce the time and resources to analyze participant transcripts?

Identify the Biggest Risks to CKD App Usage
What is the biggest risk to the success of a new CKD management app?

Improve Design Outcomes through Data-Driven Archetypes
How can we achieve an effective shared understanding of our users that is shared across Aetna Insurance users as well as CVS retail and pharmacy users?

Transgender Journey Map
What are the moments that matter to our transgender members, and how can we help them in their journey?

Make research findings available and contextually consistent
How can years of qualitative and evaluative findings be used to support ongoing development efforts?

Increase Telemedicine Adoption
What impact does education have on Telemedicine usage?

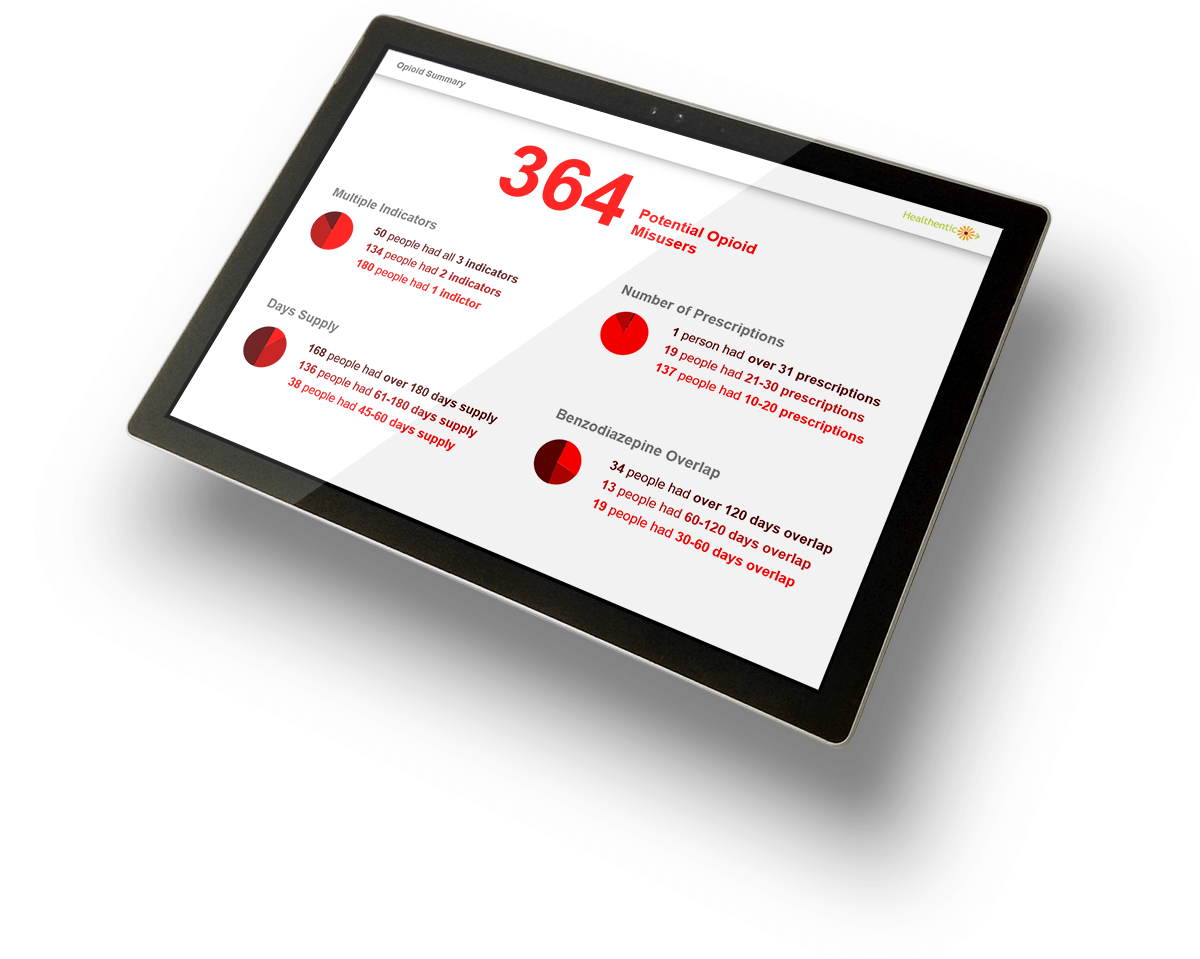
Prevent Opioid Addiction
Benefit Managers need to experience the scope of the problem, and need specific help to manage the situation.
Increase Sales of a Mental Health App
CFO sales prospects need to experience the financial impact of mental health to buy the product.

Find “Ticking Time Bomb” Patients
Employer outreach teams need the experience of better targeting at-risk members.

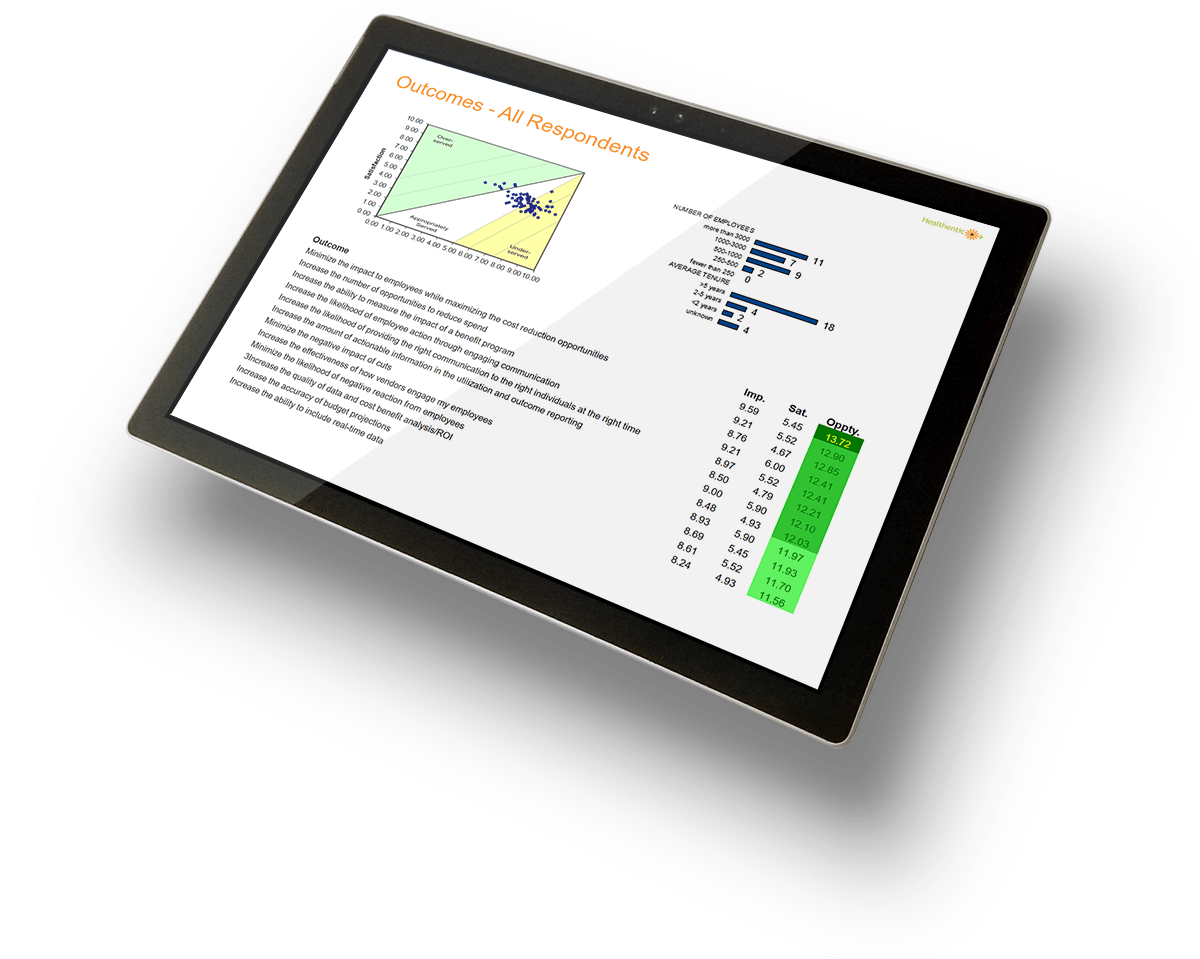
Find Benefit Manager Product Opportunities
Benefit managers need to experience easier ways to reduce cost.
Unlock Data to Improve Hospital Quality
Hospital teams need to experience more access to data to improve quality and outcomes.

Improve Claims Data Processing Throughput
Data team members need a unifying status experience while processing hundreds of claims feeds simultaneously.