Prevent Opioid Addiction
My Role
- Literature Review
- Algorithm Design
- Visual Design
- Iterative Testing
- Service Design
Summary
We were able to create a report that identified opioid misusers in claims data before they became addicted.
Problem
Benefit managers were scared. They felt helpless. What could they do facing the scope of opioid epidemic in their organization?
In 2013 we saw a disturbing increase on the number of employees taking opioid drugs in the Population Health Dashboard. It was a health issue that cost employers $25.6 billion annually.
I worked with our research team and created a white paper outlining the situation. This white paper was published in multiple sources, so it was a content marketing success. Download the White paper.
However - we needed to craft a product that could help employers better manage this dangerous situation.
Solution Overview
- Created a claims-data algorithm that identified potential misusers in claims data before they became addicted.
- Designed reporting that created a sense of urgency by highlighting the scope of the problem, and provided a de-identified list of people to put a human face on it.
- Built a consulting and data user experience that allowed Healthentic to motivate the Pharmacy Benefit managers to take action.
- Established a quality improvement reporting process to track effectiveness.
Process
- Find a way to identify employees before they became addicted.
- Create a sense of urgency for the employers.
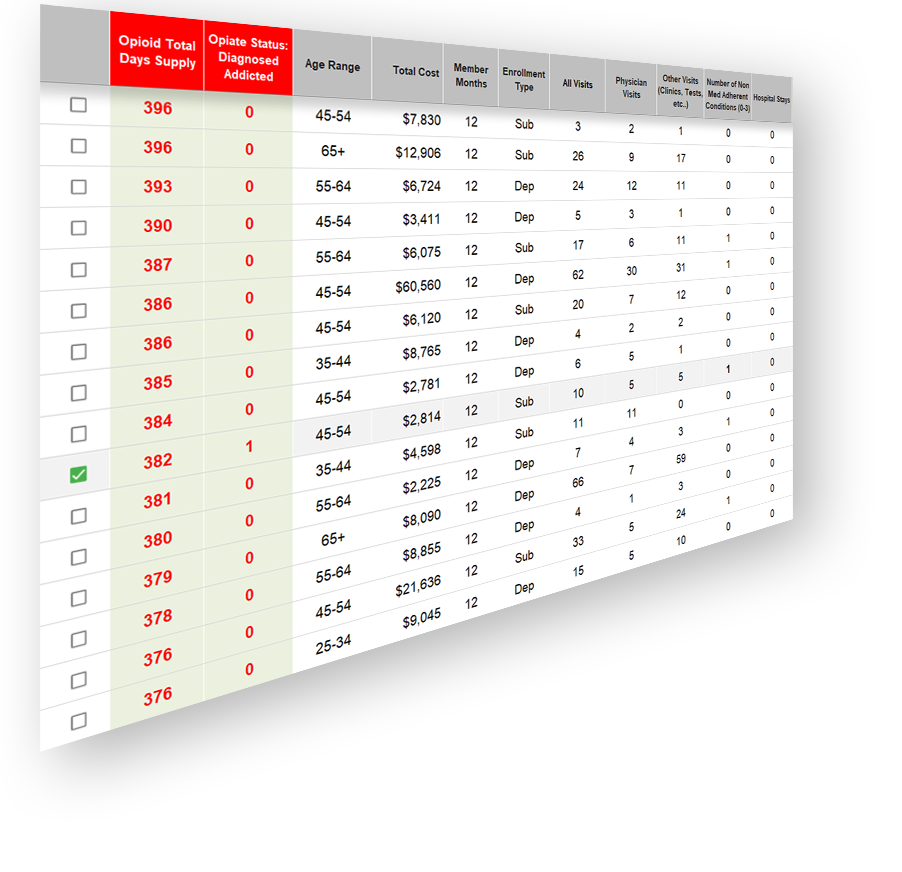
- Put a human face on the problem within the context of productive data.
- Translate that urgency into action with pharmacy benefit provider partners.
- Measure the results of that action and repeat the process.
Identify At-Risk Employees Before They Become Addicted
We needed to get in front of the problem. How could we identify early misuse?
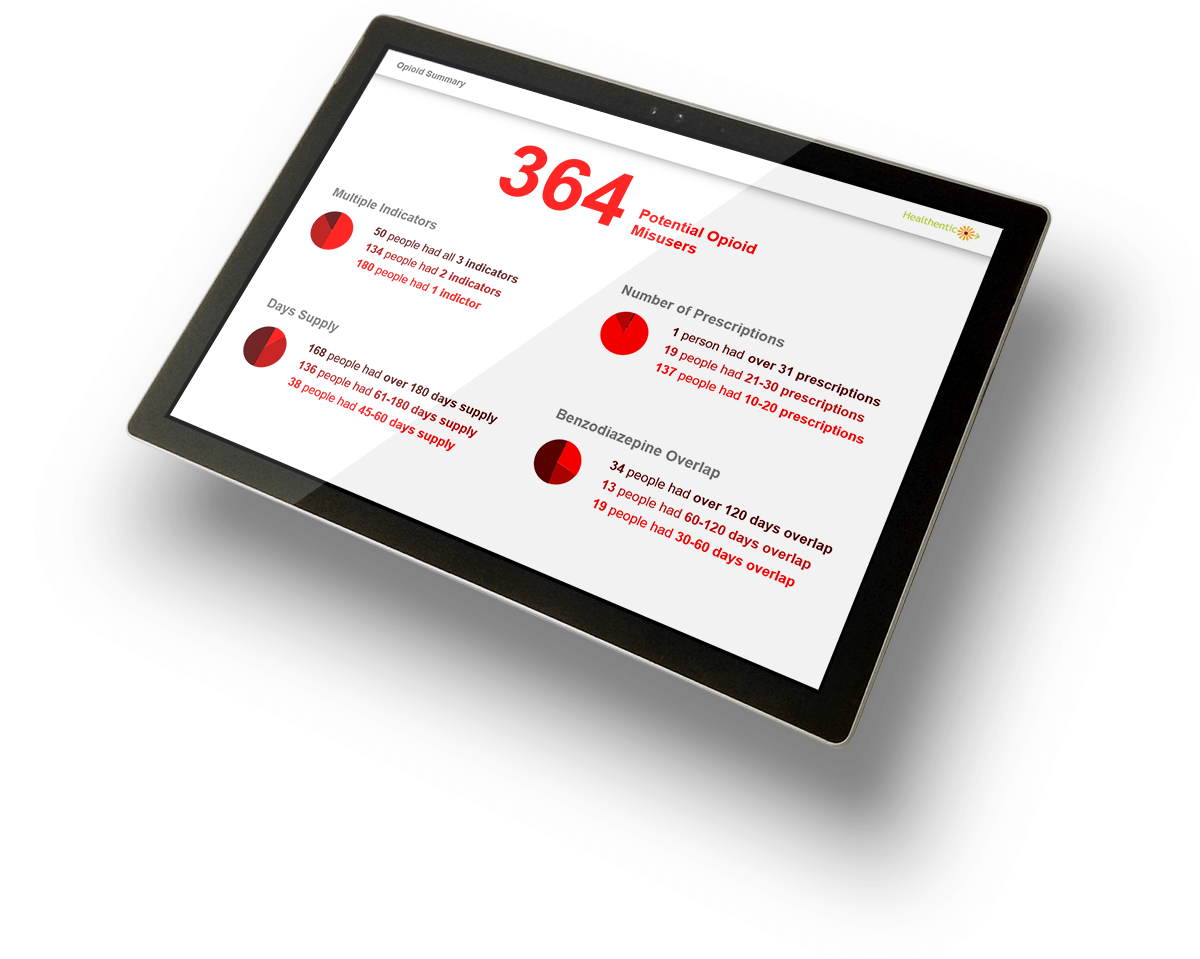
We focused on three issue flags:
- Overlapping opioid and benzodiazepine prescriptions. Benzodiazepine is a drug that enhances the opioid high and is often an indicator of misuse.
- 10 or more prescriptions.
- 120 days or greater supply dispensed. (In 2017, we changed this to 45 days based on CDC guidance.)
We needed a simple and clear report to show the scope. The summary design showed the number of potential misusers and frequency of issue flags. The experience of seeing the large number of people who had multiple issues increased urgency.
How Do we Get the Pharmacy Benefit Groups to Take Action?
After our data experience created the sense of urgency with the employer, the challenge became to address the problem with pharmacy benefit providers. They were reluctant to talk about the issue - and often dismissed requests to meet.
We found that submitting the detailed person-level report established credibility in our analysis. When the pharmacy benefit partners were sent the list of individuals it motivated them to take a meeting. At that meeting we discussed their monitoring algorithms, outreach and sometimes even reviewed deidentified case notes.
Results
- Reviewed case notes with some pharmacy benefit teams and made sure that the at-risk members were identified and part of their program.
- Found pharmacy benefit partners that were not sharing prescribing data with medical carriers - this meant that the physicians had no way of knowing which patients had opioid prescriptions. We got that fixed.
- Provided our misuse algorithms to a few of the pharmacy benefit managers so they could do a better job identifying potential misusers.
- Identified pain management clinics that were likely "pill mills" through prescribing data.