Understand Product Opportunities for the Benefit Manager Market
My Role
- Quantitative Research
- Outcomes Driven Innovation
- Qualitative Research
- Interviews
- Surveys
- Ethnographic Research
Summary
We discovered the greatest unmet needs for Benefit Managers, and the outcomes that they need.
Problem
Employers face increasing healthcare costs every year, and need ways to reduce costs with minimal impact to their employees and families.
Benefit Managers buy products and services to get jobs done. How do we build a product that will fulfill the desired outcomes of those jobs?
Solution Overview
- Discovered that the jobs with the largest opportunities involve “Engaging Employees”
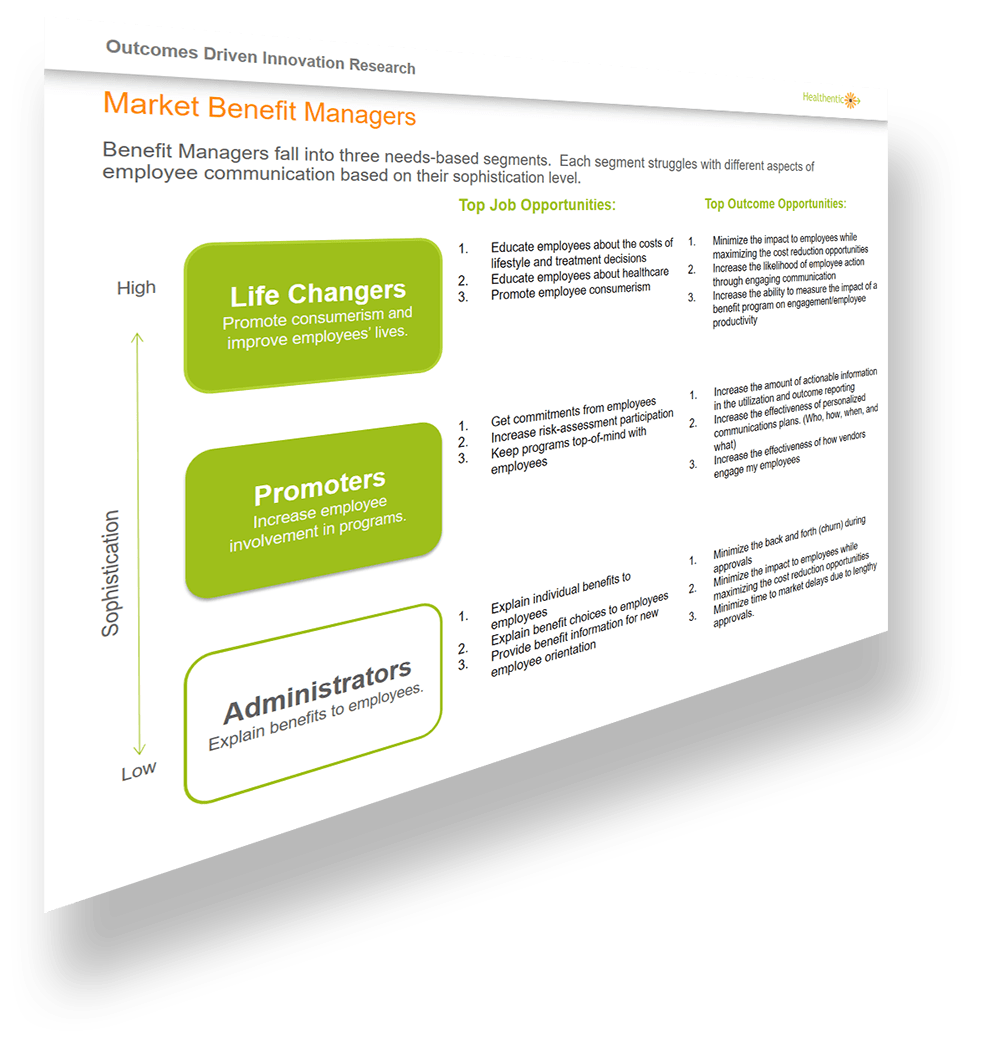
- Through cluster analysis, we found three segments that follow a sophistication model.
- The most sophisticated we called "Life Changers." These people struggle with demonstrating program successes.
- The next level was "Promoters." This group struggles to increase involvement in programs, but are not at the point of measuring them.
- The least sophisticated group were, "Administrators." They are challenged by simply explaining benefits to employees.
- I chose life changers and promoters as my target segments
- I mapped the job, “Engage Employees” and found 120 desired outcomes along nine process steps
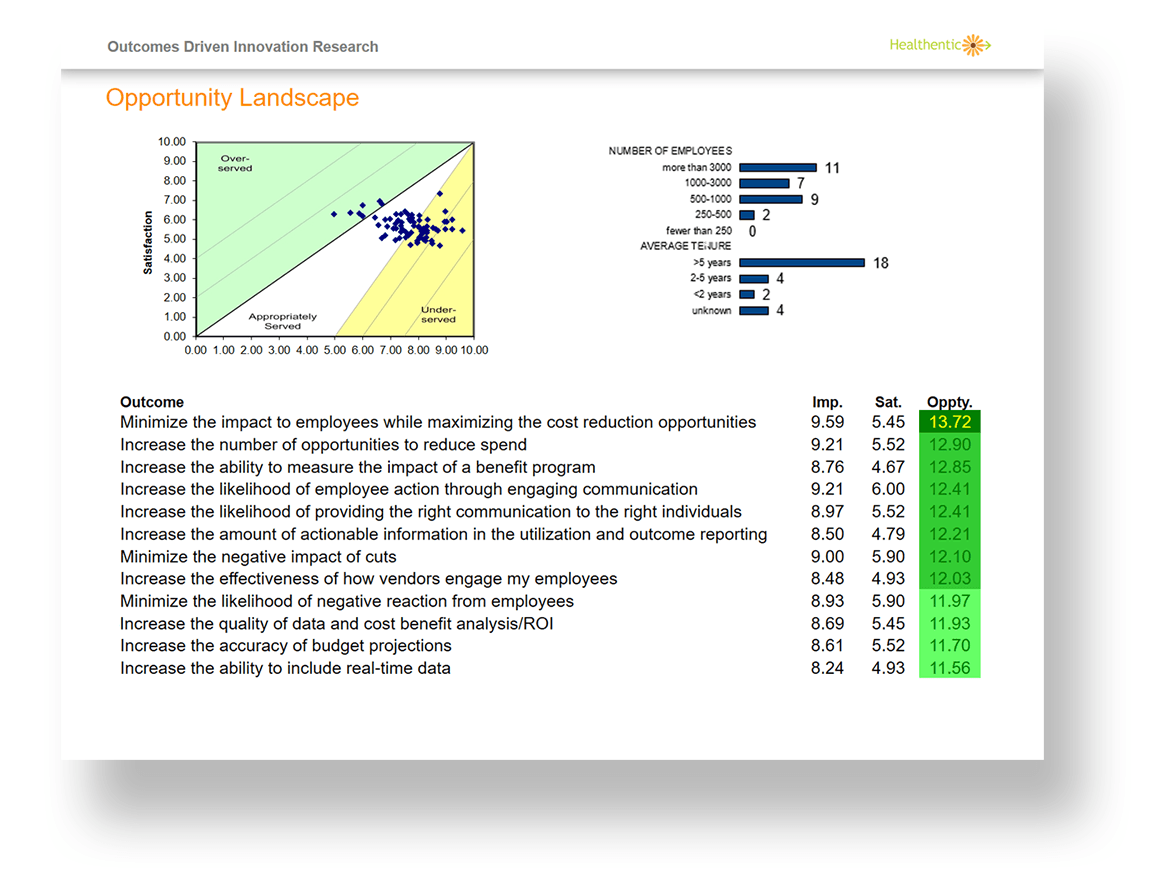
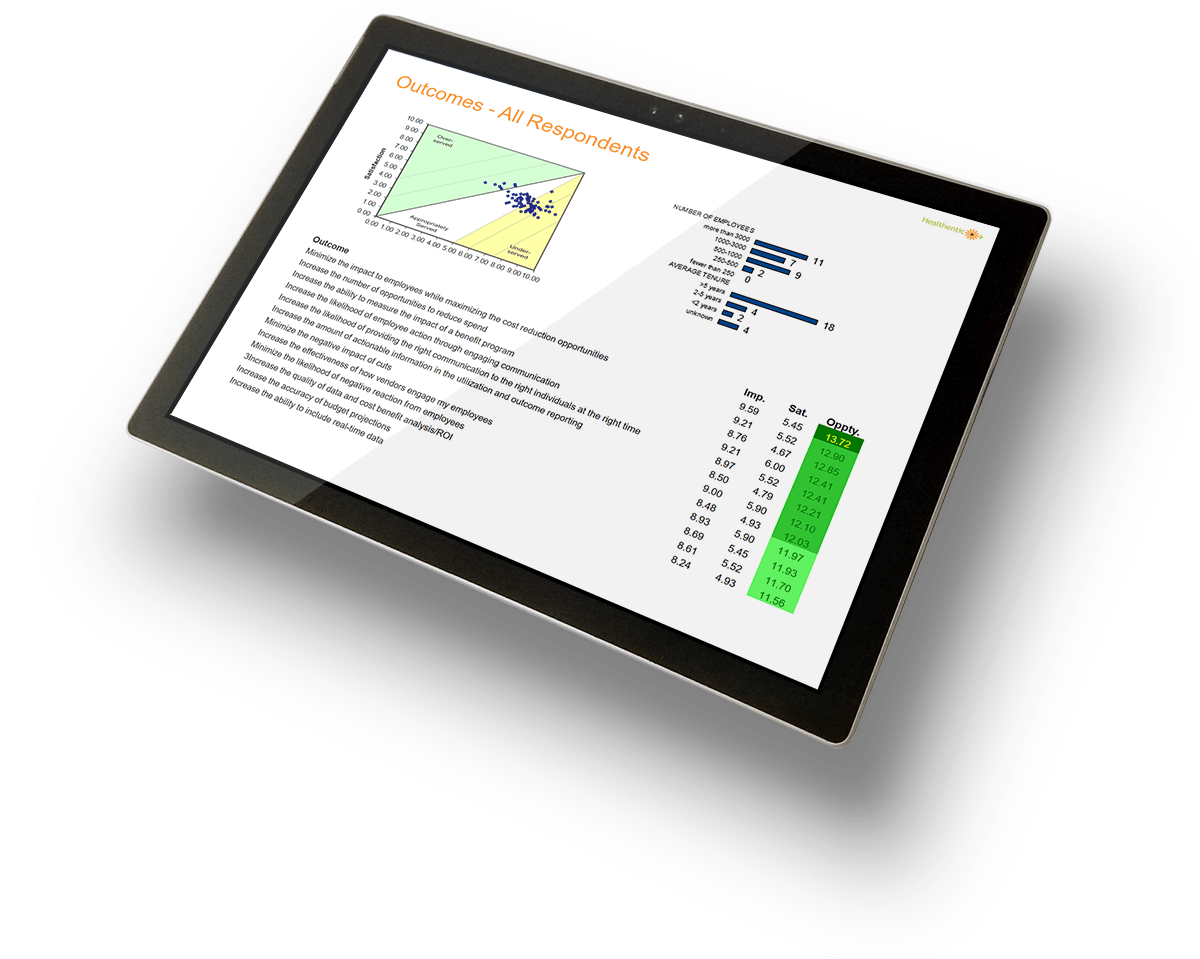
- The top three outcomes guided the development of the Population Health Dashboard:
- Minimizing impact to employees while maximizing cost reduction opportunities
- Increase the number of opportunities to reduce spend
- Increase the ability to measure the impact of a benefit program
Process
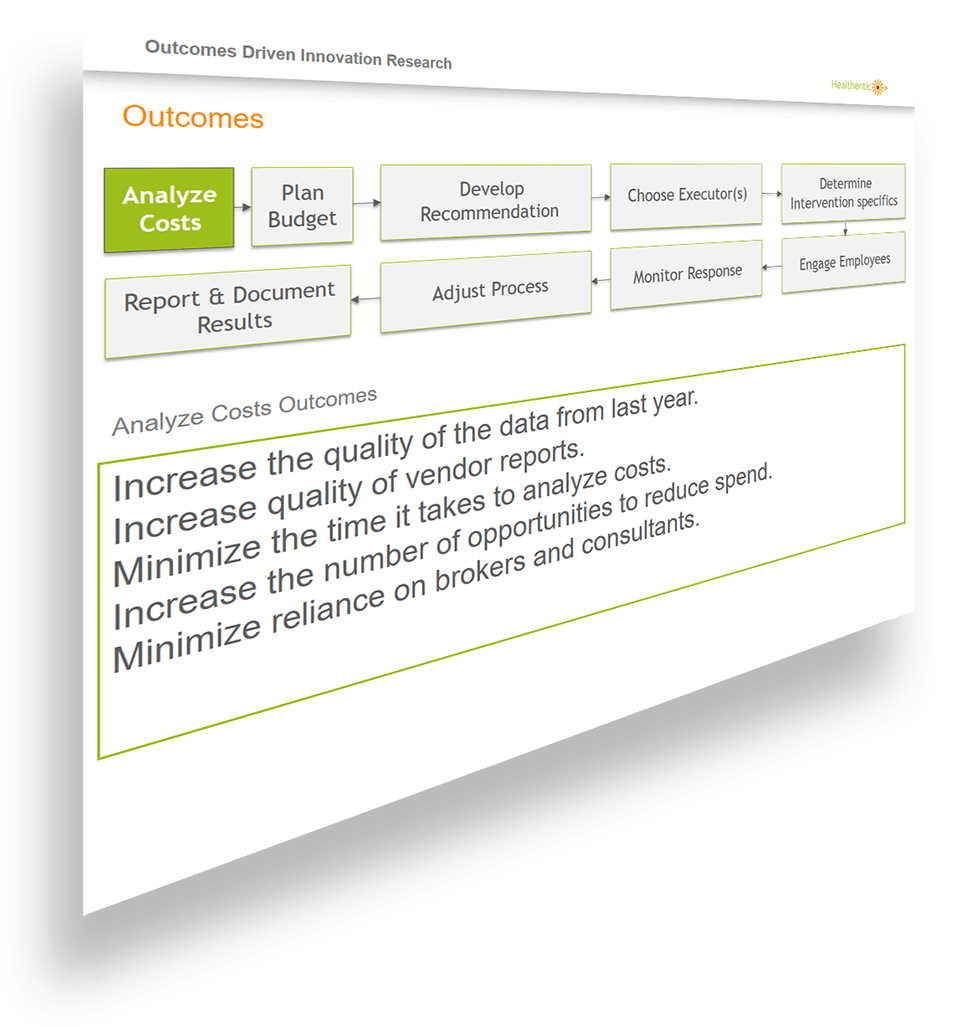
For this project I followed Stratygen’s “Outcome Driven Innovation” process. This consists of:
- Define your customers (Benefit Managers)
- Catalog all jobs that Benefit Managers do in their daily lives
- Uncover customer needs
- Cluster segments of opportunities
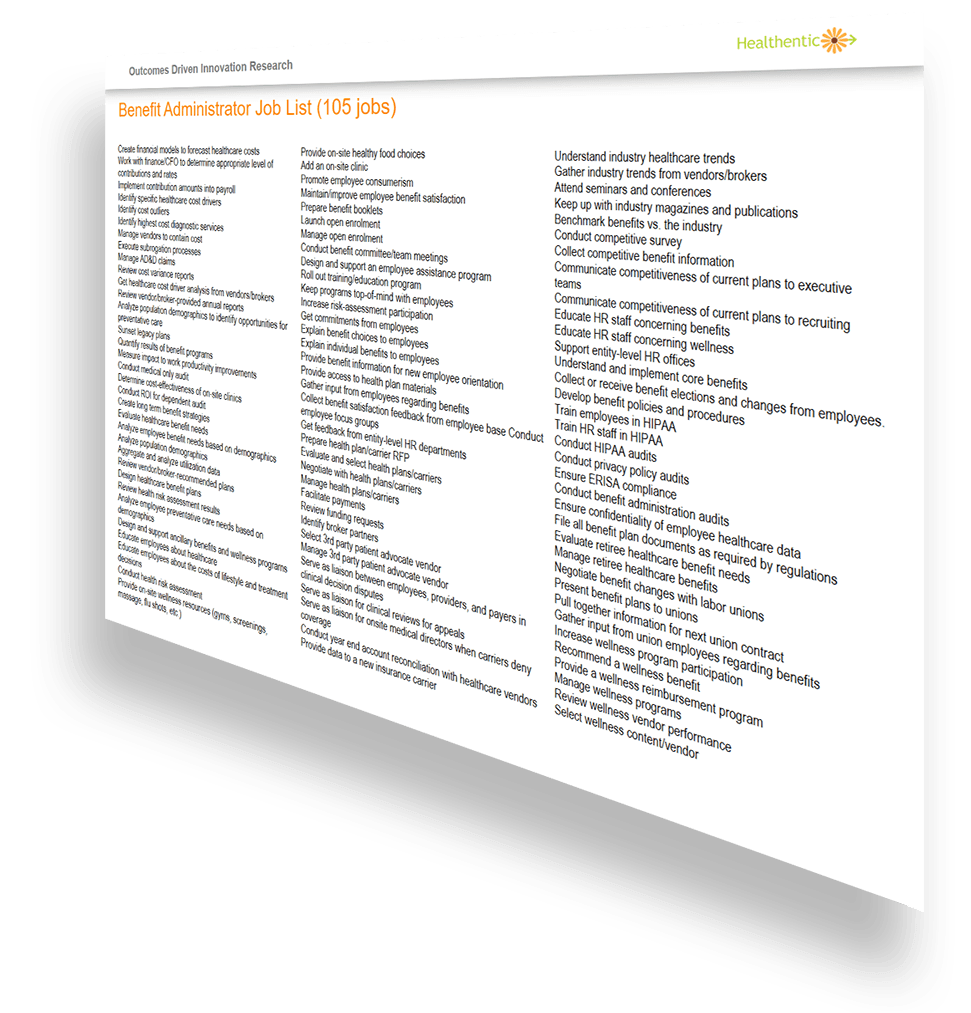
What Jobs to Benefit Managers Do?
I identified our market as Benefit Managers. These served as our “job executors”. Next, I needed to correctly determine what job they are hiring products to perform. During qualitative interviews I gathered a list of 105 jobs that Benefit Managers do as part of their role.
These jobs were listed in a quantitative survey and sent to 500 Benefit Managers. Respondents ranked each job on importance, and how satisfied they were with the ability to do those jobs. The jobs that were the greatest opportunities involved different aspects of “Engaging Employees”.
How Do Benefit Managers do this Job?
A customer need is best defined as a statement that describes how a customer measures success and value when getting a job done. These statements are the customer’s “desired outcomes”.
I conducted a set of qualitative discussion around how Benefit Managers engage employees and found a nine-step process. This became our job map. For each step I asked what were the outcomes that Benefit Managers expected.
The Opportunity Landscape
Once I had the expected outcomes, I sent another qualitative survey that asked the Benefit Managers to rank each outcome on importance, and how satisfied they were with the ability to do those jobs.
The Opportunity Landscape is a snapshot of all the customers’ needs: each dot in the landscape represents the degree to which a specific need is important to the Benefit Manger and the customer’s level of satisfaction. Jobs in the green are over-served. Jobs in the yellow are underserved.
Quotes
“Healthentic is going to put me and other consultants right out of business. A company can know at a glance how its wellness program is doing, and be deemed for validation, with no extra work except signing a form."
- Al Lewis, Author of "Cracking Healthcare Costs" and "Why Nobody Believes the Numbers"
"I think this is very powerful stuff. It’s very exciting. It's even more exciting that we can take action and save costs.”
- Dr. Philip Adamo, AVP and Medical Director, Employee Health and Occupational Injury
“This type of information took us a long time to uncover and understand. Now, in 5 seconds, the Population Health Dashboard is seeding us with suggestions. This makes it much easier for us to make benefit and wellness recommendations to every client we work with.”
- Mim Minichiello, Senior partner, HUB International
“The Wellness Decision Engine makes all my data available in one place throughout the year, and is the starting point for our wellness program.”
- Patti See, VP HR
“Healthentic has quickly become one of our most trusted and valuable partners in our corporate health promotion program!”
- Derek Kanehira, Vice President & Director of Human Resources
Results
- 57 large employers bought the Population Health Dashboard to increase the number of opportunities to reduce spend.
- 218 tracking events were captured by users in just the first two and half months of the feature launch.
- Discovered 45 opportunities with specific action plans worth an average of $622,465 per 1000 employees